
The aneurysm dome was dissected completely from the surrounding vessels. The Sylvian fissure was opened and the temporal M2 and frontal M2 were visualised. The aneurysm was approached via pterional craniotomy with the patient supine. He was maintained on Sevoflurane (1.1 MAC) and Remifentanil (0.1-0.25 mcg/kg/min). He had an uneventful intravenous induction with Propofol (150 mg), Fentanyl (100 mcg) and Rocuronium (60 mg), with Fentanyl and Propofol boluses to cover intubation and head-pin insertion. The patient was deemed to be low risk from an anaesthetic perspective. Cerebral angiography confirmed the aneurysm, and the patient was discussed in the neurovascular multidisciplinary team meeting whereby elective surgery for aneurysm clipping was offered. The scan was carried out for resection of a grade 1 myxopapillary ependymoma. The patient consented to have the details of their case published in this anonymised case report.Ī 52-year-old man presented with an incidental finding of 12 mm right MCA bifurcation aneurysm on imaging. Here, we report the case of a 52-year-old man who suffered an intra-operative PEA cardiac-arrest while undergoing elective clipping of a right MCA bifurcation aneurysm through pterional craniotomy, in the absence of an explanatory cause. The few recorded cases of intraoperative pulseless electrical activity (PEA) cardiac arrest during neurosurgery have been ascribed to medications, irrigation, coronary vasospasm, and most commonly to the trigeminocardiac reflex. Adherence to the advanced life support (ALS) algorithm may be life-saving even when the cause is unknown.Ĭase report, Aneurysm, Clipping, Neurosurgery, Cardiac arrestĬardiac arrest is an increasingly rare intraoperative complication, and relatively few cases have been reported during neurosurgery. Understanding the cause of cardiac arrest allows for prompt treatment and reversal of any precipitant, and there are specific considerations in the neurosurgical setting. We consider and discuss the alternative explanations in the literature.Ĭonclusions: Intra-operative cardiac arrest is a rare and potentially catastrophic event. No biochemical, electrophysiological, or structural abnormality was identified to explain this patient’s sudden intra-operative PEA arrest. He made a good post-operative recovery, without evidence of any new deficit. The patient was successfully resuscitated following 2 minutes of chest compressions and the administration of Adrenaline, in accordance with ALS algorithm. Proposed causes of PEA cardiac arrest in this setting include medications, irrigation, coronary vasospasm, and elicitation of the trigeminocardiac reflex.Ĭase description: Here, we report the case of a 52-year-old man who suffered an intra-operative pulseless electrical activity (PEA) cardiac-arrest while undergoing elective clipping of a right MCA bifurcation aneurysm through pterional craniotomy.
If another reversible cause has not been discovered or if the patient is known to be susceptible to hypoglycemia (e.g., brittle diabetes, past surreptitious use of insulin) then this potential cause of PEA should be considered.Background: Cardiac arrest is a rare intraoperative complication with few cases reported during neurosurgery. *Hypoglycemia is not officially one of the H’s and T’s for adults, but it still can be an important cause of PEA, especially in children. Surgical embolectomy or administration of fibrinolyticsĮCG will be abnormal based on the location of the infarction Rapid heart rate with narrow QRS complexes on the ECG Typically will be seen as a prolonged QT interval on the ECG may see neurological symptoms Rapid heart rate and narrow QRS complexes on the ECG Slow heart rate and narrow QRS complexes on the ECG difficulty breathing Typically preceded by exposure to a cold environment Peaked T waves and wide QRS complex on the ECGĬonsider calcium chloride, sodium bicarbonate, and an insulin and glucose protocol Hyperventilation consider sodium bicarbonate bolusįlat T waves and appearance of a U wave on the ECG Infusion of normal saline or Ringer’s lactateĪirway management and effective oxygenation Rapid heart rate and narrow QRS on ECG other symptoms of low volume
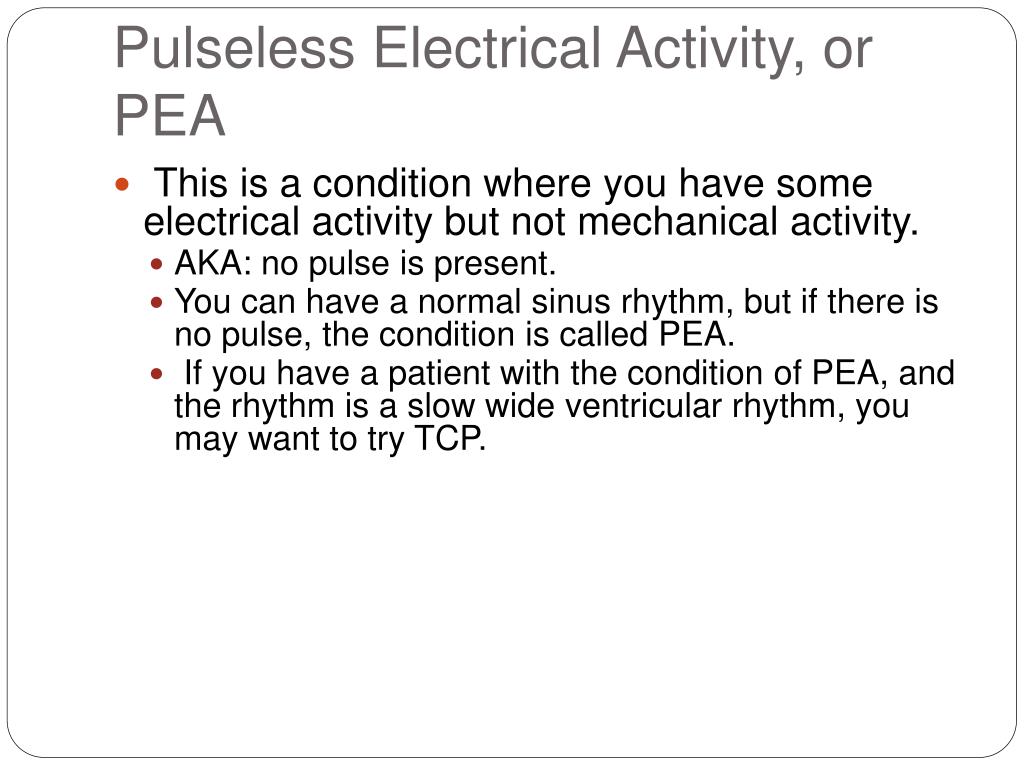
While it is important to continue to deliver compressions, ventilation, and medications according to the algorithm, it is always best to treat underlying causes of PEA and related conditions as soon as possible.


 0 kommentar(er)
0 kommentar(er)
